
Prevent varicose veins
strenuous physical activity; increased intra-abdominal pressure; constipate; Frequent pregnancies.
Conservative treatment
diet
quit smoking
Compression underwear (tights, stockings, knee socks)
Varicose veins: drug treatment
Venotonics – ointments and gels

Ointment based on the flavonoid rutin. Use an ointment containing horse chestnut extract twice daily. Gel whose active substance is an extract of grape leaves. There is also a drug capsule that can be taken twice a day on an empty stomach.
Venotonics Tablets
The saponin derivative of the drug is obtained on the basis of the horse chestnut tree, which contains the plant bioflavonoid aescin. These include medications that come in the form of drops and tablets. The most effective preparations are based on phytoflavonoids extracted from citrus fruits - a powerful intravenous supplement. Courses of these medications can last up to six months. Rutin was the first intravenous supplement. They work by improving microcirculation and have anti-inflammatory properties. Natural rutin, available in tablet and capsule form. Semi-synthetic rutin. Combined rutin. It combines a semi-synthetic derivative of rutin and ginkgo leaf extract. The drug in capsule form is taken twice daily for one month.
venous sclerosis drugs
Ointments based on acidic sulfur-containing glycosaminoglycans, glucocorticoids, and nonionic surfactants are the simplest options. However, the effect is weak and injection is required. Synthetic venous sclerosing agents. Products containing iodine or based on animal protein. These drugs are used to selectively close the small blood vessels in the area of the affected vein. Among doctors, drugs that do not cause blood clots are popular,  They only burn the wall at the level of the endothelium.
They only burn the wall at the level of the endothelium.
additional medications
Agents for improving blood microcirculation: low molecular weight dextran, purine derivatives. These drugs stimulate the breakdown of platelets, reduce blood viscosity, and increase the elasticity of red blood cells. These processes improve the blood supply to the tissue and oxidative reactions in the tissue. Anticoagulants acting directly or indirectly. Reduce the risk of thrombosis. Popular products in ointment and gel form have anti-edematous, anti-inflammatory and anti-thrombotic effects. Nonsteroidal anti-inflammatory drugs – inhibit the inflammatory process and relieve pain.
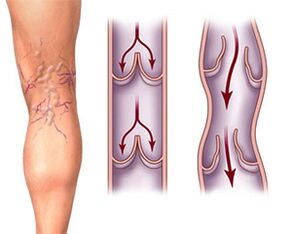
Venous Sclerosis Treatment Options
Venous sclerosis is performed before surgery to reduce the risk of postoperative thrombosis and bleeding. As an alternative to phlebotomy during surgery. The unoperated vein is closed after surgery.
puncture method
After administration, the limb is wrapped with an elastic bandage and repeated for two weeks. During the first week, the bandage will not be removed. The patient must be walking within half an hour of surgery. Patients should elevate their limbs when sleeping every day, avoid sitting or standing for long periods of time, and avoid walking a lot.

















